Andrew Gregory, Health editor in Chicago, Sun 4 Jun 2023 13.00 BST
Taking the drug osimertinib once a day after surgery reduces chance of patients dying by 51%, trials show

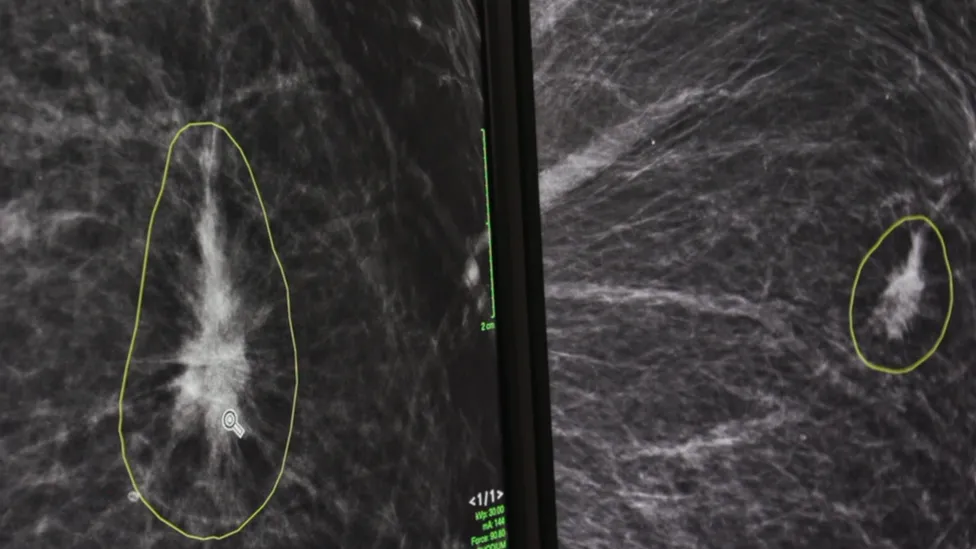
The survival benefit of osimertinib ‘was observed consistently’ in an analysis across all study subgroups, the study says. Photograph: utah778/Getty Images/iStockphoto
A pill taken once a day cuts the risk of dying from lung cancer by half, according to “thrilling” and “unprecedented” results from a decade-long global study.
Taking the drug osimertinib after surgery dramatically reduced the risk of patients dying by 51%, results presented at the world’s largest cancer conference showed.
Lung cancer is the world’s leading cause of cancer death, accounting for about 1.8 million deaths a year. The results of the late-stage study, led by Yale University, were presented at the American Society of Clinical Oncology’s (Asco) annual meeting in Chicago.
“Thirty years ago, there was nothing we could do for these patients,” said Dr Roy Herbst, the deputy director of Yale Cancer Center and lead author of the study. “Now we have this potent drug."
“Fifty per cent is a big deal in any disease, but certainly in a disease like lung cancer, which has typically been very resistant to therapies.”
The Adaura trial involved patients aged between 30 and 86 in 26 countries and looked at whether the pill could help non-small cell lung cancer patients, the most common form of the disease.
Everyone in the trial had a mutation of the EGFR gene, which is found in about a quarter of global lung cancer cases, and accounts for as many as 40% of cases in Asia. An EGFR mutation is more common in women than men, and in people who have never smoked or have been light smokers.
Speaking in Chicago, Herbst said the “thrilling” results added huge weight to earlier findings from the same trial that showed the pill also halves the risk of a recurrence of the disease.
Herbst, the assistant dean for translational research at Yale School of Medicine, said the pill was proven to be “practice-changing” and should become the “standard of care” for the quarter of lung cancer patients worldwide with the EGFR mutation.
Some patients in the UK, US and other countries are already able to access the drug, he said, but more should benefit.
Not everyone diagnosed with lung cancer is tested for the EGFR mutation, which needs to change, Herbst said, given the study’s findings. “This further reinforces the need to identify these patients with available biomarkers at the time of diagnosis and before treatment begins.”
Treatment after surgery with osimertinib, also known as Tagrisso and made by AstraZeneca, “significantly lowered” the risk of death in lung cancer patients, the trial results reported. “Adjuvant osimertinib demonstrated an unprecedented, highly statistically significant and clinically meaningful overall survival benefit in patients,” the report said.
After five years, 88% of patients who took the daily pill after the removal of their tumour were still alive, compared with 78% of patients treated with a placebo. Overall, there was a 51% lower risk of death for those who received osimertinib compared with those who received placebo.
The survival benefit “was observed consistently” in an analysis across all study subgroups, including those with stage one, stage two and stage three lung cancer. Chemotherapy had been given to 60% of those in the study, and the survival benefit of osimertinib was seen regardless of whether prior chemotherapy was received.
“It is hard to convey how important this finding is and how long it’s taken to get here,” said Dr Nathan Pennell, an Asco expert who was not involved with the study. “This shows an unequivocal, highly significant improvement in survival.”
Angela Terry, the chair of EGFR Positive UK, a lung cancer charity, said the findings were “very exciting” and “hugely significant”.
“A five-year overall survival rate of 88% is incredibly positive news,” she said. “Having access to a drug whose efficacy is proven and whose side-effects are tolerable means patients can be confident of and able to enjoy a good quality of life for longer.”
https://www.theguardian.com/science/202 ... ling-study